Alveoli
Microscopic air sacs in lungs for gas exchange
Alveoli are tiny, sac-like structures within the lungs that serve as the primary site for gas exchange between the air and the bloodstream. Each lung contains millions of alveoli, providing a vast surface area for efficient oxygen and carbon dioxide exchange. These microscopic air sacs are surrounded by a dense network of capillaries, allowing close contact between air and blood. The alveoli have thin walls composed of simple squamous epithelium, which facilitates rapid diffusion of gases. They are lined with a fluid containing surfactant, which reduces surface tension and prevents collapse during exhalation.
Location
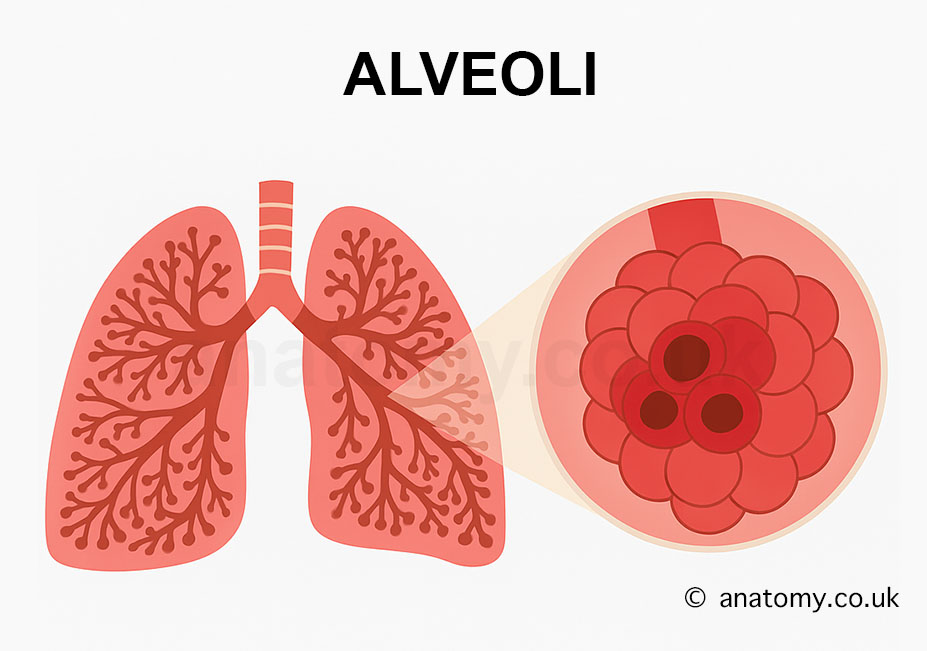
Alveoli are located at the terminal ends of the respiratory bronchioles within the lungs. They form clusters known as alveolar sacs, which branch out from the bronchioles in the lower respiratory tract. These sacs are found deep inside the lungs, embedded within the lung tissue, and are positioned near capillary networks to allow for efficient gas exchange.
Anatomy
Structure of Alveoli
Alveoli are microscopic, balloon-like structures that are specialized for gas exchange in the lungs. Each alveolus has a hollow, sac-like shape surrounded by a dense capillary network. The walls of the alveoli are extremely thin, allowing for efficient diffusion of gases. They are grouped into alveolar sacs, which are clusters of alveoli connected to each other through alveolar ducts. The alveoli are supported by a network of elastic fibers, which enable them to expand during inhalation and recoil during exhalation. This elasticity is crucial for maintaining airflow and pressure within the lungs.
Alveolar Walls (Alveolar Septa)
The walls of the alveoli, also known as alveolar septa, are made up of three main layers:
Epithelial Layer – Composed of two types of cells, type I pneumocytes and type II pneumocytes.
Basement Membrane – A thin layer that provides structural support and separates the epithelial cells from the capillary network.
Capillary Network – Surrounds the alveoli, enabling gas exchange by bringing blood into close contact with the alveolar air.
Cell Types in Alveoli
Type I Pneumocytes
Flat, thin cells that form about 95% of the alveolar surface area.
Responsible for creating the thin diffusion barrier required for gas exchange.
Provide structural integrity to the alveolar walls.[6]
Type II Pneumocytes
Cuboidal cells that make up about 5% of the alveolar surface area.
Secrete surfactant, a lipoprotein substance that reduces surface tension, preventing alveolar collapse during exhalation.
Capable of dividing and differentiating into type I pneumocytes for repair and maintenance of the alveolar walls.
Alveolar Macrophages (Dust Cells)
Specialized immune cells present within the alveoli.
Phagocytose (engulf and digest) inhaled particles, pathogens, and debris to maintain cleanliness and prevent infections.
Interalveolar Septa
The alveoli are separated by interalveolar septa, which contain:
Capillaries for gas exchange.[4]
Connective tissue with collagen and elastic fibers, providing structural support and elasticity.
Pores of Kohn, which are small openings between adjacent alveoli that allow for collateral ventilation and equalization of air pressure.
Alveolar Capillary Interface
The alveoli are surrounded by a dense network of capillaries that facilitate gas exchange. This interface, also known as the respiratory membrane, is approximately 0.5 microns thick and consists of:
Alveolar Epithelium – Thin lining of type I pneumocytes.[1]
Fused Basement Membranes – A shared layer between the alveolar and capillary walls that minimizes the diffusion distance.
Capillary Endothelium – The inner lining of capillaries through which gases diffuse into the blood.
Blood Supply
The alveoli are richly vascularized by the pulmonary circulation:
Pulmonary Arteries bring deoxygenated blood from the heart to the alveoli.
Pulmonary Veins carry oxygenated blood back to the heart for systemic distribution.
Nerve Supply
The alveoli are primarily regulated by the autonomic nervous system:
Parasympathetic Nerves stimulate bronchoconstriction and mucus secretion.
Sympathetic Nerves promote bronchodilation, increasing airflow.
Lymphatic Drainage
Lymphatic vessels around the alveoli drain excess fluid and immune cells, maintaining fluid balance and preventing pulmonary edema. The lymph drains into bronchopulmonary lymph nodes at the hilum of the lung.
Microscopic Features
Under a microscope, the alveoli reveal:
Thin Squamous Epithelium for rapid diffusion of gases.
Surfactant Layer produced by type II pneumocytes, forming a thin film to stabilize the alveoli.
Elastic Fibers around alveoli, allowing expansion and recoil.
Macrophages scattered within the lumen, maintaining alveolar hygiene.[8]
Function
Primary Site of Gas Exchange
The alveoli are the primary site for gas exchange in the lungs, enabling oxygen to enter the bloodstream and carbon dioxide to be expelled.
Oxygen Uptake – Oxygen from inhaled air diffuses across the thin alveolar walls into the surrounding capillaries, binding to hemoglobin in red blood cells for transport to tissues.
Carbon Dioxide Removal – Carbon dioxide, a waste product from cellular metabolism, is transported via blood to the alveoli, where it diffuses into the alveolar space and is exhaled.
Diffusion Process – This exchange occurs due to the concentration gradient, as oxygen is higher in alveolar air and lower in blood, while carbon dioxide follows the opposite gradient.
Maintenance of Gas Concentration
The alveoli continuously maintain optimal oxygen and carbon dioxide levels in the blood.
During inhalation, alveoli receive fresh oxygen-rich air.
During exhalation, they expel carbon dioxide-rich air, maintaining balance and supporting cellular metabolism.
Surfactant Secretion
Alveoli are lined with type II pneumocytes that secrete pulmonary surfactant, a substance critical for:
Reducing Surface Tension – Prevents alveolar collapse during exhalation by lowering the surface tension within the alveoli.[7]
Improving Compliance – Enhances the flexibility and expansion of alveoli, allowing them to fill easily during inhalation.
Preventing Fluid Accumulation – Helps keep alveoli dry and prevents fluid buildup, maintaining effective gas exchange.
Elastic Recoil and Ventilation Support
Alveoli are surrounded by elastic fibers that contribute to their ability to expand and contract.
Expansion During Inhalation – The elastic fibers stretch, allowing alveoli to fill with air.
Recoil During Exhalation – The fibers return to their original shape, aiding in expelling air without requiring active muscle contraction.
This elastic property ensures efficient ventilation and minimizes energy expenditure during breathing.
Collateral Ventilation
Alveoli are interconnected by pores of Kohn, allowing air to flow between neighboring alveoli.
Pressure Equalization – Prevents alveolar collapse by balancing pressure across different regions of the lungs.
Alternative Airflow Pathways – Maintains ventilation even if some airways are blocked, ensuring uninterrupted gas exchange.[5]
Defense Against Pathogens
Alveoli play a critical role in immune defense by removing harmful particles and pathogens.
Alveolar Macrophages – Specialized immune cells that engulf and digest bacteria, dust, and debris, preventing infections.
Mucociliary Clearance – Mucus and cilia in the upper airways trap particles before they reach the alveoli, reducing exposure to contaminants.
Immune Response Activation – Macrophages release signals to recruit additional immune cells when infections occur.
Regulation of Blood pH
Alveoli indirectly help regulate blood pH by controlling carbon dioxide levels.
Carbon Dioxide and pH Balance – High carbon dioxide levels lower blood pH (acidosis), while low levels raise it (alkalosis).
Respiratory Compensation – The alveoli adjust ventilation rates to remove or retain carbon dioxide, maintaining pH within the normal range (7.35–7.45).[3]
Facilitating Vocalization
Alveoli contribute to vocalization by providing the air pressure needed for phonation.
Air expelled from the alveoli passes through the larynx and vibrates the vocal cords to produce sound.
Variations in airflow support speech modulation and singing.
Oxygen Storage and Reserve
Alveoli act as temporary oxygen reservoirs, ensuring a continuous supply of oxygen even between breaths. This reserve capacity becomes particularly important during activities like exercise or holding breath, where oxygen demand fluctuates.
Support for Pulmonary Circulation
The alveoli maintain pulmonary circulation efficiency by facilitating rapid gas exchange across the thin respiratory membrane.[2] Blood flow and ventilation are matched (ventilation-perfusion coupling) to optimize oxygen uptake and carbon dioxide removal.
Clinical significance
The alveoli are vital for gas exchange, and any damage or dysfunction can lead to severe respiratory conditions. Pneumonia, an infection causing inflammation and fluid buildup in the alveoli, impairs oxygen absorption and leads to breathing difficulties. Acute respiratory distress syndrome (ARDS) results from alveolar damage due to trauma, infection, or inhalation of toxic substances, causing severe hypoxia. Emphysema, a form of chronic obstructive pulmonary disease (COPD), involves the destruction of alveolar walls, reducing surface area for gas exchange and leading to breathlessness. Pulmonary edema, caused by fluid accumulation in the alveoli, interferes with oxygen diffusion and may result from heart failure. Neonatal respiratory distress syndrome (NRDS) occurs in premature infants due to insufficient surfactant production, causing alveolar collapse. Diagnosis of alveolar disorders often involves chest X-rays, CT scans, or pulmonary function tests, while treatments range from oxygen therapy and ventilation support to medications and rehabilitation programs.
Last updated on May 17, 2025