P
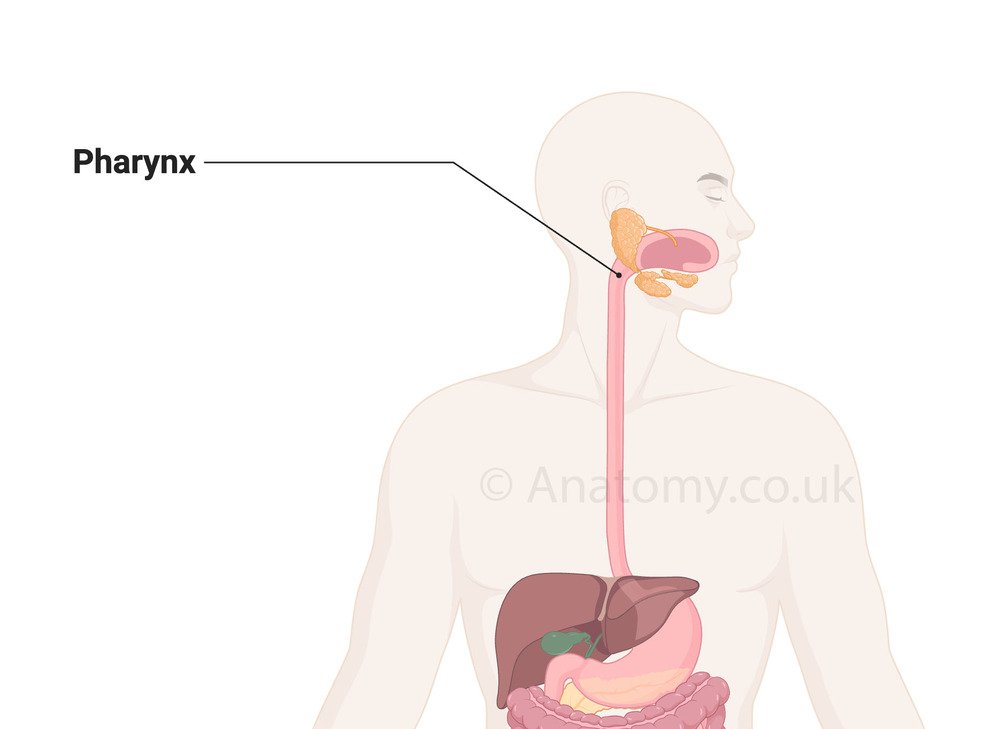
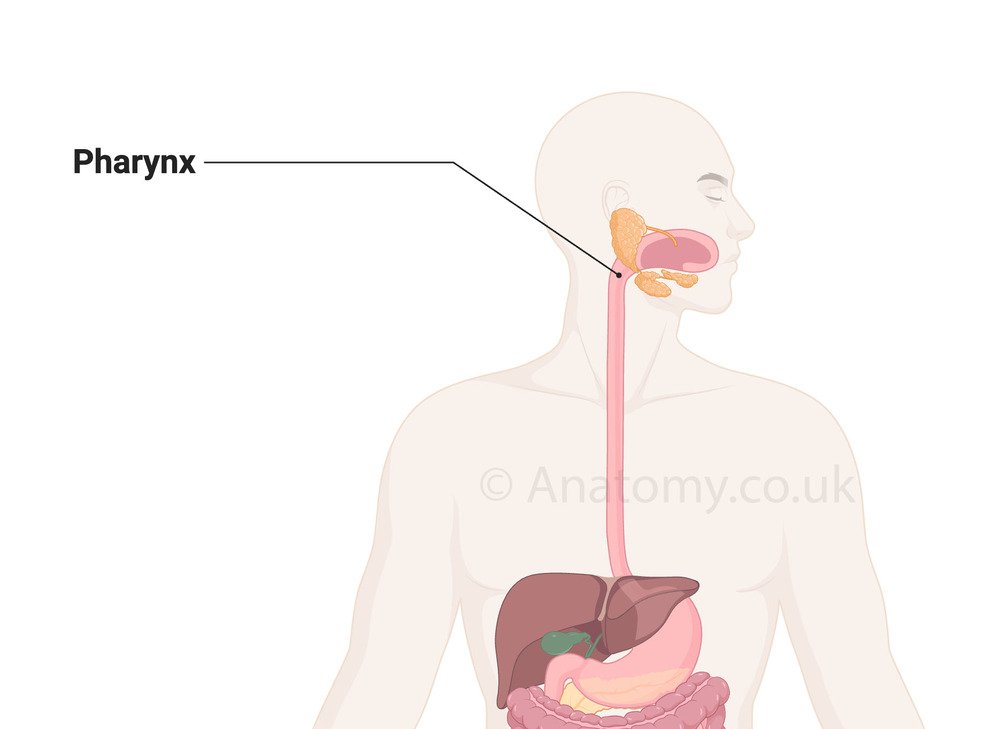
Pharynx
Muscular tube connecting nasal cavity to esophagus
RegionHead and Neck
SystemDigestive System
The pharynx is a muscular tube that serves as a shared pathway for both the respiratory and digestive systems. It connects the nasal cavity and oral cavity to the larynx and esophagus, facilitating the passage of air, food, and liquids. The pharynx is divided into three regions: the nasopharynx, oropharynx, and laryngopharynx, each with distinct anatomical features.
Location
The pharynx is located in the head and neck region, extending from the base of the skull to the level of the sixth cervical vertebra (C6). It lies posterior to the nasal cavity, oral cavity, and larynx and anterior to the cervical spine.Anatomy
The pharynx is a funnel-shaped muscular tube that forms a critical part of both the respiratory and digestive systems. It is approximately 12–14 cm in length and extends from the base of the skull to the level of the sixth cervical vertebra (C6), where it continues as the esophagus. Below is a detailed description of its anatomy:Regions of the Pharynx
The pharynx is divided into three anatomical regions:Nasopharynx
Location: The uppermost part of the pharynx, lying posterior to the nasal cavity and superior to the soft palate. Boundaries:- Superior: Base of the skull (sphenoid and occipital bones).
- Inferior: Soft palate.
- Contains the pharyngeal tonsil (adenoids) on its posterior wall.
- The opening of the auditory (Eustachian) tube is located on its lateral walls, surrounded by the torus tubarius.
- The pharyngeal recess is a small depression behind the torus tubarius.
Oropharynx
Location: The middle part of the pharynx, posterior to the oral cavity and inferior to the nasopharynx. Boundaries:- Superior: Soft palate.
- Inferior: Upper border of the epiglottis.
- Anterior: Posterior surface of the tongue.[8]
- Contains the palatine tonsils between the palatoglossal and palatopharyngeal arches.
- Communicates with the oral cavity through the oropharyngeal isthmus.
Laryngopharynx (Hypopharynx)
Location: The lowest part of the pharynx, posterior to the larynx. Boundaries:- Superior: Upper border of the epiglottis.
- Inferior: Continuous with the esophagus at the level of the cricoid cartilage (C6).
- The piriform recesses are located on either side of the laryngeal inlet, guiding food and liquids into the esophagus.
- Lies anterior to the cervical vertebrae.
Musculature of the Pharynx
The pharynx is composed of two layers of muscles:- Outer Circular Layer (Constrictor Muscles): Includes the superior, middle, and inferior pharyngeal constrictors, which contract sequentially during swallowing to propel food into the esophagus.
- Inner Longitudinal Layer: Includes the stylopharyngeus, palatopharyngeus, and salpingopharyngeus muscles, which elevate and shorten the pharynx during swallowing and speech.[6]
Pharyngeal Wall Layers
The pharyngeal wall is made up of several layers from internal to external:- Mucosa: Lined with ciliated pseudostratified columnar epithelium in the nasopharynx and stratified squamous epithelium in the oropharynx and laryngopharynx.
- Submucosa: Contains connective tissue, blood vessels, and lymphatics.
- Muscular Layer: Includes the circular and longitudinal muscles.
- Fibrous Layer (Pharyngobasilar Fascia): Thick superiorly, anchoring the pharynx to the base of the skull.
- Adventitia (Buccopharyngeal Fascia): Outermost connective tissue layer, containing nerves and blood vessels.
Vascular Supply
Arterial Supply: Supplied by branches of the external carotid artery, including:- Ascending pharyngeal artery.
- Facial artery (ascending palatine and tonsillar branches).
- Maxillary artery.
- Superior thyroid artery.
Lymphatic Drainage
Lymph drains into the deep cervical lymph nodes, particularly the jugulodigastric node near the angle of the mandible, which is significant for tonsillar drainage.Nervous Supply
The pharynx receives both motor and sensory innervation via the pharyngeal plexus: Motor Innervation: Primarily supplied by the vagus nerve (cranial nerve X), except for the stylopharyngeus (supplied by the glossopharyngeal nerve, cranial nerve IX). Sensory Innervation:- Nasopharynx: Maxillary nerve (V2 branch of the trigeminal nerve).
- Oropharynx: Glossopharyngeal nerve (cranial nerve IX).
- Laryngopharynx: Vagus nerve (cranial nerve X).
Anatomical Relations
- Anteriorly: Related to the nasal cavity, oral cavity, and larynx.
- Posteriorly: Lies against the cervical vertebrae (C1–C6) and prevertebral fascia.
- Laterally: Related to the carotid sheath, containing the internal carotid artery, internal jugular vein, and vagus nerve.
Function
The pharynx is a vital structure in the human body, serving as a shared pathway for the respiratory and digestive systems. Its functions are integral to swallowing, breathing, speech, and immune defense. Below is a detailed explanation of its roles:Passageway for Air and Food
The pharynx functions as a dual-channel, allowing the passage of air to the respiratory system and food to the digestive system:- Airway Function: Air passes through the nasopharynx and oropharynx on its way to the larynx and trachea.[1]
- Food Passage: Food and liquids travel from the oropharynx to the laryngopharynx and into the esophagus.
Swallowing (Deglutition)
The pharynx plays a central role in the complex process of swallowing, which occurs in three phases: Oral Phase (Voluntary):- The tongue pushes the bolus of food into the oropharynx.
- The pharynx begins preparing to coordinate swallowing by opening the oropharyngeal isthmus.
- The pharyngeal constrictor muscles contract sequentially (superior to inferior), propelling the bolus from the oropharynx to the esophagus.
- The longitudinal pharyngeal muscles elevate and shorten the pharynx, creating space for the bolus.
- The nasopharynx is sealed off by the elevation of the soft palate, preventing food from entering the nasal cavity.
- The epiglottis folds over the laryngeal inlet to direct the bolus away from the airway.
Speech and Voice Resonance
The pharynx contributes to the modulation of sound and resonance in speech:- Acts as a resonating chamber, amplifying and modifying sound produced by the vocal cords in the larynx.[7]
- The shape and tension of the pharyngeal walls influence voice quality and clarity.
- The oropharynx and nasopharynx work together to direct airflow during speech for proper articulation.
Immune Defense
The pharynx houses lymphoid tissues that are part of the body’s immune system:- Pharyngeal Tonsil (Adenoids): Located in the nasopharynx, it captures and destroys inhaled pathogens.
- Palatine Tonsils: Positioned in the oropharynx, these guard against ingested or inhaled pathogens.
- Lingual Tonsil: Found at the base of the tongue, it provides immune protection for substances entering through the oral cavity.
Equalization of Pressure in the Middle Ear
The nasopharynx contains the openings of the auditory (Eustachian) tubes, which connect the middle ear to the pharynx:- The pharyngeal muscles, particularly the salpingopharyngeus, help open these tubes during swallowing or yawning, allowing air to flow into the middle ear.
- This function equalizes pressure across the tympanic membrane (eardrum), preventing barotrauma and maintaining optimal hearing.[5]
Breathing Regulation
During respiration, the pharynx ensures proper airflow: The nasopharynx remains open to allow unobstructed passage of air to the trachea. The soft palate prevents air from escaping into the oral cavity during nasal breathing.Protection Against Aspiration
The pharynx protects the airway during swallowing:- The soft palate prevents food or liquid from entering the nasal cavity.
- The epiglottis and closure of the vocal cords block food from entering the trachea, reducing the risk of aspiration.
Coordination with Reflexes
The pharynx plays a role in important reflexes: Gag Reflex:- Triggered by stimulation of the pharyngeal mucosa, preventing foreign objects from entering the throat.[3]
- Controlled by the glossopharyngeal nerve (cranial nerve IX) and the vagus nerve (cranial nerve X).
Maintenance of Airway Patency
The pharyngeal muscles stabilize the pharyngeal walls, preventing collapse during breathing, particularly during sleep or heavy respiration.Clinical Significance
The pharynx is a vital structure involved in swallowing, breathing, and speech, and its dysfunction can lead to various clinical conditions:- Dysphagia (Difficulty Swallowing): Disorders affecting the pharynx or its muscles (e.g., neurological diseases like stroke or ALS) can impair swallowing, causing food or liquids to enter the airway, increasing the risk of aspiration pneumonia.
- Obstructive Sleep Apnea (OSA): Weakness or collapse of the pharyngeal walls during sleep can obstruct airflow, causing apnea, snoring, and daytime fatigue.
- Tonsillitis and Adenoid Hypertrophy: Infections or enlargement of the tonsils or adenoids can cause difficulty in breathing, swallowing, or hearing (due to Eustachian tube blockage).
- Pharyngeal Tumors: Cancers of the pharynx (e.g., nasopharyngeal carcinoma) can cause symptoms like dysphagia, nasal obstruction, or ear pain.[2]
- Zenker’s Diverticulum: Weakness in the pharyngeal wall, particularly at Killian’s triangle, can result in pouch formation, leading to regurgitation and halitosis.
Published on January 7, 2025
Last updated on April 24, 2025
Last updated on April 24, 2025